When the small remote community of Binjari went into lockdown late last year, the Northern Territory’s emergency Covid plans kicked in hard.
Police set up a roadblock at the turnoff 18km south-west of Katherine. Nobody was allowed in or out. Defence personnel arrived to deliver food and essentials to people in their homes. Floodlights were installed at the edges of the community and stayed on all night, apparently to deter escapers. Residents reported drones flying overhead, checking they were obeying the stay-at-home orders.

Sitting outside her house in Binjari, Wardaman woman Olivia Raymond recalls how scared people were by the lockdown measures, as much as the virus itself.
“There was police here walking around the community, and the police over there on the oval, watching over, making us feel like … an invasion. Yeah, it was heavy.”
Binjari is small. About 300 Wardaman and Jawoyn people live there, and it doesn’t have a police station.
The floodlights shone in the windows all night and kept everyone awake, Raymond says.
“It was like in a movie or something. We never had sleep because there was one light over here, one light there, and we had drones that flew around, watching the community, even though there was a lot of police along the main road.”
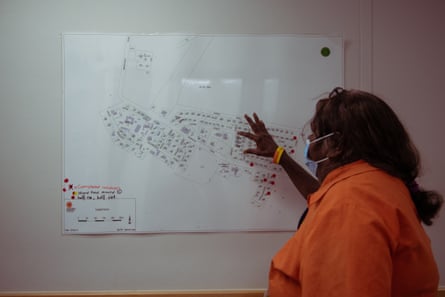
Raymond is on the board of the Wurli-Wurlinjang health service, which covers Binjari and other “closeup” communities to Katherine. She says she understood the measures were supposed to control the spread of the virus, but the force of the lockdown frightened people.
“I think there was about five people who wanted to run away that night, because they couldn’t stand it,” she says.
Then the crazy rumours started. Family members began sending her links to Facebook videos in which people were claiming Binjari residents were being forcibly removed from their homes by the army, forcibly quarantined, forcibly vaccinated. None of it was true.

NT chief minister at the time, Michael Gunner, lost his temper at the misinformation being circulated by what he called “tinfoil hat-wearing tossers, sitting in their parents’ basements in Florida”.
The chief executive of Binjari Community Aboriginal corporation, Deb Aloisi, says she was getting emails and phone calls every day from anti-vaxxers here and overseas. She spent a lot of time trying to explain that the community was not being mistreated. In the end, she says, she just stopped answering the phone.
Eventually, Binjari elders had to issue a public statement declaring the rumours false.
“We are in lockdown because we’re in the biggest fight of our lives. We’re trying to keep safe,” they wrote. “We’re trying to do the right thing by the community and Katherine. We don’t appreciate outside people making comments that are untrue. People on social media saying that our people are being mistreated need to realise their comments are hurting the very people they claim to care about.”
In early December, an elderly woman from Binjari became the first person in the Northern Territory to die of Covid. While there were many other hospitalisations, there was no other loss of life at Binjari.

The Wurli-Wurlinjang Health services chief executive, Peter Gazey, said the emergency response plan worked well – at first.
“The defence force were there handing out the meals, not attacking people. It was all really well done,” Gazey says.
“The problems were the houses. Some of them, because people were visiting, had up to 20 people so there was no way they could isolate and stop the spread.”
Wurli has a client base of about 5,000 people, many of them with early-onset chronic health conditions who live in run-down and overcrowded homes. Binjari hasn’t had any new houses, or renovations of existing homes, for 20 years, Gazey says.
There have been five new houses built at Binjari since 2017, but the lockdowns made it clear that almost all the properties are overcrowded or in need of essential repairs.
“During the lockdown one house had 20 people in it, because they’d come from Timber Creek, and then they were stuck in town with family. It does fluctuate when there’s funerals or business going on, people travel around. Houses that normally have four people can have 15 people,” Gazey says.
The Binjari outbreak peaked before Christmas. Covid is still a major problem in the region, but Wurli-Wurlinjang is now facing the health issues sidelined during the pandemic. Some of them are noticeably worse.
“Childhood immunisations have dropped off, they haven’t been as well attended. Diabetes hasn’t been attended to. People’s blood sugars are higher, there have been more hospitalisations and treatment because of that. With kidney disease we’ve found people are now more end-stage,” Gazey says.

Fatigue follows trauma
The heat and humidity are fierce in the Top End in late January, the wet season.
At Lajamanu, a Warlpiri community eight hours’ drive south-west of Katherine, it’s usually 30C by 9am, and can easily reach the mid-40s during the day.
When Covid was detected in the wastewater at Lajamanu in late January, Katherine West health service sent a team to test every resident, roughly 700 people.
The plan was to swab everyone, do a follow-up at five days, and then a third round of testing two weeks later. In all, more than 2,100 swabs.

The conditions for everyone were terrible, the chief executive of Katherine West, Sinon Cooney, says.
“When we were going house to house to identify who was positive and who their contacts were, we were counting houses with 15 adults and 15 kids in them. And these are three or four-bedroom houses with no air conditioning, in the wet season – just absolutely horrific conditions for people,” Cooney says.
“In some of our communities, the majority of houses were in isolation. So our whole workforce had to be reoriented to that, regardless of their program area. We had to send all of our staff from town out bush, swabbing in full PPE in 45 degrees.”
David McGuinness is the public health manager at Katherine West, but in February he was part of the emergency team in Lajamanu.
McGuinness spent three years as a nurse in disaster and war zones in South Sudan, Myanmar, Yemen and Pakistan, working for Doctors Without Borders. He says the environmental conditions were like those he’d experienced overseas.
The heat made it impossible to work for more than 45 minutes at a time.
“You could see people’s sweat pooling up in the elbows of their gown that they were working in even after that long. Some of the gowns were a little bit more breathable than others, but some of the gowns completely held all the water inside, and you would look over at someone swabbing and there’d be like a cup of water in their elbow,” he says.
“The NT in the buildup [to the wet season] is quite a difficult place to be [even] when you’re not in full PPE. We were doing that for 12 or more hours a day.”
The full PPE kit was an N-95 Mask, a full-length gown, an eye shield, a hair net and two sets of gloves “because in the heat, if you take off a set of gloves, you can’t get another set back on because your hands are so wet. So you have a mid-layer glove which you’re sanitising instead.”
The Lajamanu school bus was the “cool-off spot”, where the air conditioning was left on full-blast.

“It wasn’t really possible to walk around the whole community in the heat, so you would do a few houses and then come back, doff your PPE, jump on the bus with the aircon on, drink water and cool down, while another team would go to the next few houses. And then you just rotate around that way.”
The team did that for 16 days.
“There are a few things you learned, like not to put sunscreen on your forehead, because in the sun, the sweat would just run into your eyes. A few people had quite irritated eyes from sunscreen running into their face,” he says.
Quick GuideHow to get the latest news from Guardian Australia
Show

Email: sign up for our daily morning and afternoon email newsletters
App: download our free app and never miss the biggest stories
Social: follow us on YouTube, TikTok, Instagram, Facebook or Twitter
Podcast: listen to our daily episodes on Apple Podcasts, Spotify or search "Full Story" in your favourite app
“It was the long days which were really the hardest part. Once you swabbed everyone, you needed to make sure everything was labelled and bagged up. A lot of the team wouldn’t get to bed until midnight, and then up at about six to do it all again. I was definitely having swabbing dreams.”
McGuinness says about 450 swabs had come back negative and they were getting ready to scale down the team, thinking the wastewater detection may have been a false alarm.
“Then the last 100 swabs came back, and one of them was positive. Everyone was literally packing their bags and we said, “hold up, we’re going to have to swab everyone again, just to make sure that that person hasn’t passed it on to anybody”.”

During the outbreak, Sinon Cooney estimates they had 750 cases, or about a third of the population, with Covid which Katherine West managed without its usual cohort of nursing staff.
Many nurses come to the NT from interstate or overseas, particularly New Zealand, on Fifo contracts. Cooney says they depend on the same nurses coming back year after year, who have the skills and experience to manage the needs of remote communities. Border closures meant the workforce was seriously depleted for two years, and local staff are yet to recover.
Cooney says in the bush “you recruit for emergency skills … because if someone walks into a clinic clutching their chest, you need to know what to do. If there’s a motor vehicle accident, you need to know how to manage that.
“[Covid] has really demonstrated the resilience of our staff on the ground in the bush. But I think the other thing is the real acuity of our response. For the last two years, people have had their foot on the gas, and they were working really hard. Now, things have eased off a bit, we’re returning to some sense of normal, people are really tired and just wanting a break. It’s still a struggle,” Cooney says.

Fatigue has followed trauma. But Covid has not abated significantly, according to John Paterson, the head of the NT’s Aboriginal community-controlled health organisations, AMSANT.
“We’re not out of the woods, so to speak. We’re still seeing alarming death rates, from January 1 this year until now,” Paterson says.
“We’re not comfortable with the current statistics and infections that are going on, and we need governments to not forget about Covid, but to be vigilant. If we start to see a spike in numbers we’d be very supportive of those governments and the health leadership to take the appropriate course of action to get on top of it.”
Ultimately, Paterson says, Covid will remain a problem as long as Aboriginal families in remote communities live in poor and overcrowded housing, which is at the heart of every chronic health condition they are fighting to contain.

“Everybody understands that housing is linked to health. If you have good housing with toilets operating, showers functioning, electricity, then you can bet your bottom dollar that there will be reasonably good health,” he says.
“The pandemic definitely exposed the big gap in the overcrowding of housing. How can you expect people to go and self-isolate, undertake all the hygienic and public health measures that we’re being advised of, when you’ve got 20 to 30 people already residing in a three bedroom house that’s got one toilet, electrical cables hanging out of the roof and walls, the ceiling’s all asbestos and they’re just uninhabitable?
“Get the politicians to come out and live for a two-week period on Centrelink benefits in the most remote, harshest communities and let them experience the lifestyle that people are currently experiencing,” Paterson says.
Lorena Allam’s work is supported by the Balnaves Foundation